
TORONTO—As their U.S. neighbors to the south plow full-speed ahead in reopening their economy and reclaiming the life they had before coronavirus, most Canadians remain sheltered at home in lockdown, wondering when it will ever be their turn to get a shot in the arm.
The health care system in the country’s most populous province, Ontario, is groaning under the weight of a third wave deadlier than anything yet seen in the pandemic. Life-flight helicopters evacuate ICU patients from hot spots in Toronto to rural medical centers on a daily basis in an attempt to release pressure from overburdened urban hospitals.
The public Medicare system, available to all, is bending but hasn’t broken. No one is going without care, and not a single hospital bill has been issued anywhere in the country. But vaccination continues to be a glaring weak spot.
As of this writing, official Government of Canada data show that just over 24% of the population have received at least one dose (compared to 43% in the U.S. and 51% in the U.K.). When it comes to percentage of people fully vaccinated, Canada records only 2.37% (compared to the U.S.’s 30% and Britain’s 20%).
Despite billions of dollars worth of advance vaccine purchases made by Justin Trudeau’s government in 2020—before any clinical trials were even completed—repeated factory delays and nationalistic blockades by other countries have left Canada falling further behind its developed peers in vaccinations.
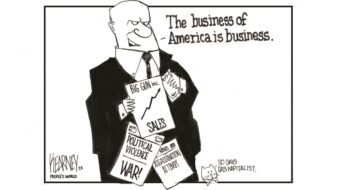
But the origins of the vaccine shortfall are not just recent. Also to blame are shortsighted efforts by successive past governments to privatize and sell off the country’s domestic vaccine production capacity, along with the refusal of pharmaceutical corporations to invest research and development dollars into a system that prizes affordable generic medicines over the unlimited patent-protected profits of capitalist health care.
Public health success, private health failure
Given the reputation of Canada’s free public health care system among American liberals, many in the U.S.—if they pay any attention to goings-on in the North at all—have been surprised to learn the country is struggling. To be sure, outside of getting jabs in arms, the health system has performed well during the coronavirus crisis.
Throughout the pandemic, Canada consistently had far lower rates of infection and death than the U.S. Paradoxically, absent a vaccine, that means Canada is actually more susceptible to trouble now than the U.S., simply because so many more Americans have had coronavirus than have Canadians.

“It’s a gift and a curse that we’ve had reasonable control of our COVID-19 pandemic throughout the last few months,” Dr. Zain Chagla, infectious disease physician at McMaster University in Hamilton, told the press last week. “The reality is there’s estimates of 25% of Americans being infected at some point or another,” he said. “In Canada, the figure is probably closer to the 10% range, so we are nowhere near a population-based herd immunity.”
In major U.S. cities, a combination of mass infection and, now, mass vaccination means that more people have antibodies—something resembling herd immunity is being reached.
Anticipated deliveries and promises from manufacturers could see Canadian supply pick up soon, but at the moment, most people still have no idea when they’ll eventually be able to sign up. Skepticism also remains high, as previously scheduled vaccine arrivals have been repeatedly canceled or seen the number of doses slashed.
The thing that separates Canada from faster-vaccinating countries like the U.S. and the U.K. is that it lacks the ability to manufacture its own COVID shots at home. Instead, it remains totally reliant on foreign supplies. It wasn’t always this way. For decades, Canada was actually a world leader in vaccine development and production.
One hundred years ago this year, Frederick Banting and Charles Best, researchers at the University of Toronto, discovered insulin, a life-saving treatment for diabetes. The formula was licensed to manufacturers around the world, denying any one company the ability to monopolize profits and earning the finders a Nobel Prize. It helped launch Connaught Labs, which became a leading producer of not just insulin, but also the smallpox vaccine and others.
Premised on such a service mission, Connaught was never a very profitable company and was nationalized by the Canadian government of Pierre Trudeau (the current prime minister’s father) in the 1970s. Ironically, once it became a publicly owned company, the lab was pressured to start turning a profit—which it just couldn’t do, given the high costs of research and development.
Once the Conservatives came to power, the lab was sold off. Its massive production facility in Toronto was privatized in the late 1980s, and what’s left of it is owned by French pharma giant Sanofi. Another Canadian vaccine factory in Montreal, the Institut Armand Frappier, was similarly put on the auction block in the 1990s. It was bought by British-based GlaxoSmithKline. When COVID struck, neither facility could be easily converted to producing for the pandemic, and a joint effort by the two companies to develop a coronavirus vaccine came to nothing.
Canadian government attempts to entice another company to make coronavirus vaccines in the country—particularly AstraZeneca—were refused. Dr. Earl Brown, a virology expert at the University of Ottawa, says this is likely due to the country’s public health policy, which favors cheaper generic drug manufacturers over profit-focused companies.
Canada isn’t perceived by the pharma giants as a place to make big money, whereas other countries provide stronger profit-protecting patent guarantees. Thus, many multinational companies keep their investment in the Canadian market limited—a consequence of the country’s decision to prioritize people over profits.
Worsening the situation have been the “vaccine blockades” enacted by many nations—including the United States. The “America First” policy inherited from Trump has, for the most part, carried over into the new Biden administration. Only recently has the U.S. government begun authorizing the sale of some surplus stockpiles (usually of brands not yet approved by the FDA) to other nations.

As soon as Pfizer and Moderna’s vaccines were approved, for instance, the U.S. government immediately bought up all scheduled production for months into the future and entirely banned exports. The hoarding has benefitted the U.S. population when it comes to vaccine availability, but at a terrific financial cost to the public coffers. Getting vaccines from producers has so far been a case of money talks and everything else walks. The U.S. is generally paying 25-75% more per dose than are E.U. countries. It’s reminiscent of the early days of the pandemic when mysterious U.S. government officials would show up at overseas airports with suitcases full of cash and suddenly planes loaded with test supplies would be re-routed to America from their previous destinations.
Lessons learned?
The Trudeau government is attempting to deal with the crunch by rushing construction of a new publicly owned vaccine factory with the capacity to turn out 250,000 shots per month—but it won’t be operational until November at the earliest. In the meantime, the country is left to the vagaries of the private pharma companies, which have generally failed to meet agreed delivery schedules.
The pandemic has exposed the steep costs of privatization and profiteering—not just in financial terms, but also in lives lost. The neoliberal policies of the 1980s and ’90s have come back to haunt the leaders of today. Some, like the federal Trudeau government, appear to have learned a lesson and claim they’ll build the industrial health infrastructure needed for the future. Others, like the Conservative provincial government in Ontario, continue to flail about, unable to implement a distribution system capable of getting the few vaccines that are available to those who need them most.
As for the vaccine nationalism and profit-driven global pharmaceutical system, it guarantees that the rest of the world’s people will have to stand in line to escape the pandemic, possibly for years. And for many countries, like India, the wait will be much deadlier than for Canadians, who at least have a robust universal health care system to help them cope.











Comments